Diabetes and the eye Introduction
Diabetes is a major worldwide health concern affecting almost 10% of the adult population and continuing to rise. People with diabetes often have disease in the eye called diabetic retinopathy (DR). Diabetic retinopathy is the most frequent complication of diabetes and occurs due to prolonged periods of elevated blood sugar levels. The blood vessels providing nutrition to the retina become damaged by the high sugar content in the blood, leading to leakage (swelling) or blockage of the vessels (reduced blood supply meaning less oxygen and nutrient delivery), and ultimately visual impairment and blindness. Diabetic retinopathy is important as it is the leading cause of blindness in the working-age population and is largely preventable.
Risk factors for Development of DR
- Duration of Diabetes – the longer a person has diabetes, the greater the risk
- Poor control of the following 3 factors has been shown to accelerate the progression of DR
- Blood sugar levels
- Blood pressure
- Cholesterol
- Smoking
- Pregnancy – in some cases, pregnancy may lead to rapid progression of diabetic retinopathy. Close monitoring is recommended during pregnancy.
What are the symptoms?
Symptoms are usually minimal until the patient has advanced disease, therefore regular checks by the optometrist (in early stages) or ophthalmologist (when things start to get serious) is strongly recommended to identify disease early and ensure treatment is started in a timely manner.
Symptoms which you may notice include
- Blurred vision and difficulty focusing
- Distortion (straight lines can appear wavy or objects can appear bigger or smaller)
- Floaters
- Loss of vision (sudden or gradual)
How is it Diagnosed?
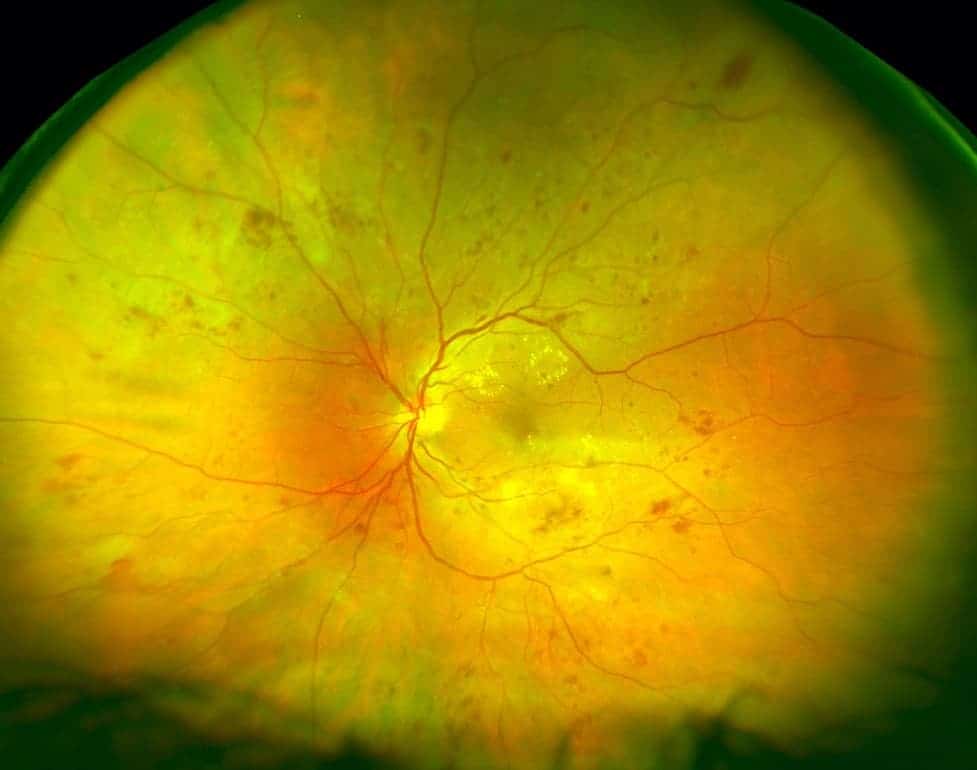
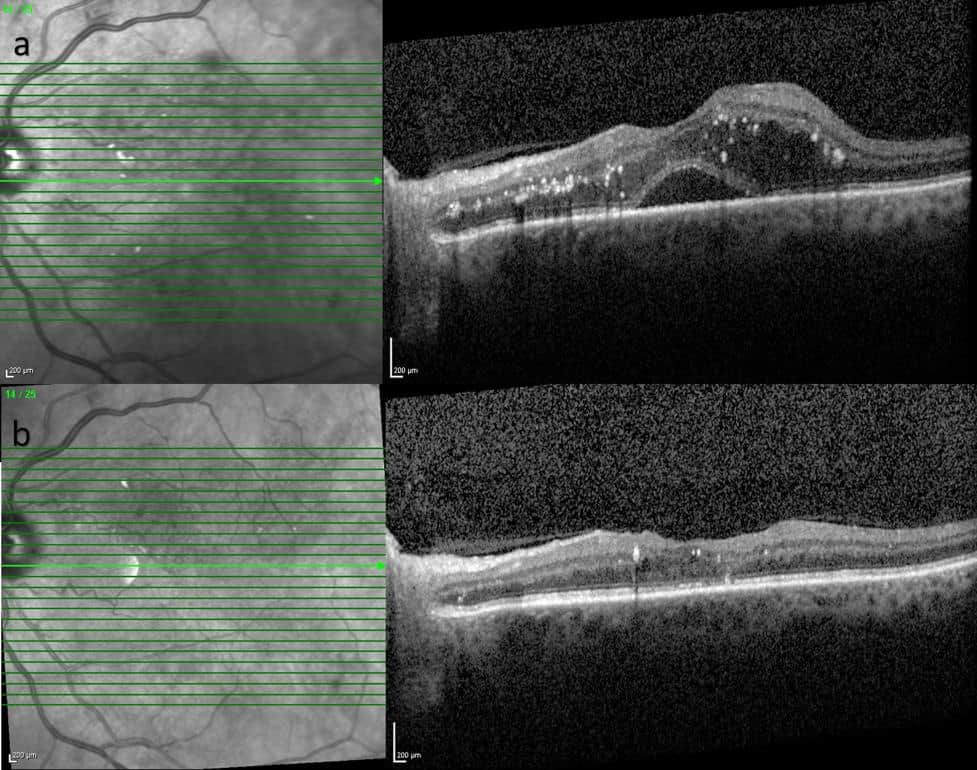
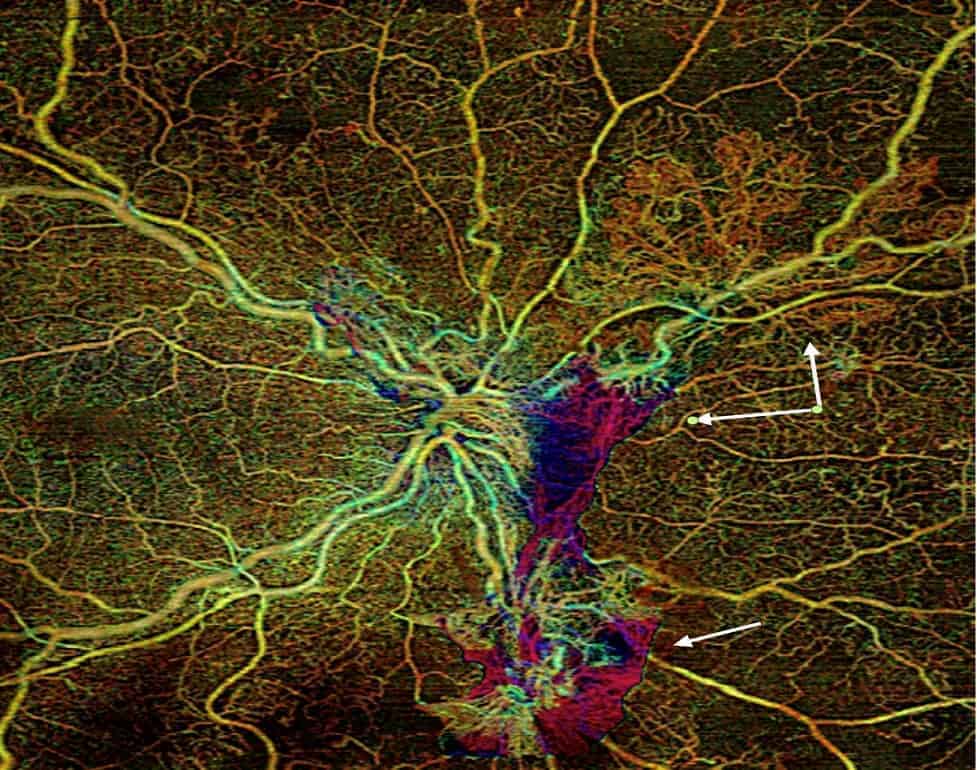
Your pupils will be dilated in order to thoroughly assess the retina which is like photographic film in the camera in the back of the eye. Investigations may be performed including photography, OCT (laser scans), OCTA (a laser-guided assessment of the blood supply) or fluorescein angiography (a photographic test with a special dye). These tests help the doctor assess the severity, check for progression of disease, and monitor response to treatment.
TYPES of DIABETIC RETINOPATHY
Diabetic retinopathy is generally split into two categories, Diabetic Maculopathy and Diabetic Retinopathy – both can cause visual loss independently or in combination.
- Diabetic Maculopathy
This the most common cause of visual impairment for diabetics. Damage to the tiny blood vessels supplying the macula (the central part of the retina that serves your fine central vision) leads to either swelling(termed Diabetic Macular Oedema, or ‘DMO’) or vessel blockage resulting lack of oxygen and nutrient delivery (termed MacularIschaemia). Ultimately these can cause temporary or permanent blurring of central vision.
- Diabetic Retinopathy
This describes the damage to blood vessels supplying oxygen and nutrition to the peripheral retina. As disease progresses, various signs on retinal examination are used to grade the severity. The most advanced stage is Proliferative Diabetic Retinopathy (PDR) and this is the most common cause of visual loss and blindness in younger patients with Type 1 Diabetes. This severe form of diabetic retinopathy indicates extensive blockage of peripheral blood vessels resulting in growth of abnormal blood vessels to compensate for the lack of oxygen. These fragile blood vessels often bleed causing sudden loss of vision or the scar tissue that accompanies them can result in nasty retinal detachments.
Treatment
Treatment may be required once the Diabetic Maculopathy or Diabetic Retinopathy reaches a certain level. Several treatments are available, and a combination of these may be employed to ensure the best possible outcome
- Laser– lasers can be used in the office to treat some patients with DMO and PDR. Macular laser for DMO is painless and aims to reduce the leakage and swelling at the macula but has been largely overtaken by intravitreal injections. Peripheral retinal laser treatment (termed ‘panretinal photocoagulation’) for PDR makes the abnormal new blood vessels shrivel up and reduce the chance of bleeding and retinal detachment.
- Intravitreal injections of ‘anti-VEGF’ medications such as Lucentis, Eylea, Beovu and Avastin; or steroid medications such as triamcinolone or Ozurdex – if the vision is reduced due to swelling of the macula (DMO), intravitreal injections can be very effective in reducing the swelling and improving the vision. They can also prevent the growth of new blood vessels described above (neovascularisation). The injections are performed with a very fine needle and local anaesthesia to make the eye numb and are usually very well tolerated. These revolutionary treatments have been a minor miracle in terms of the outlook for patients with these (and other) retinal conditions, and can effectively reduce the swelling, reduce the risk of further deterioration, and often result in significantly improved vision, particularly if disease is detected early. Monthly injections are typically required initially, with the interval extended over time, and potentially ceasing after a number of years in many diabetic patients.
- Surgery – in severe cases where loss of vision from extensive bleeding or retinal detachment has occurred, surgery is required. The surgery aims to clear the blood from the eye or fix the retinal detachment, recovering some vision and allowing for other treatments such as laser or injections to proceed in the future.
What Can You Do?
To help slow the development and progression of diabetic retinopathy and vision loss, patients are advised to:
- Optimise blood sugar control and other cardiovascular factors such as blood pressure and cholesterol levels. Aim for HbA1c (which is the long term blood sugar test ordered by your GP or endocrinologist) under 7%.
- Stop smoking, exercise regularly, and maintaining a healthy weight
- Attend regular eye checks, as early detection is key
- If you have visual symptoms, see your eye specialist promptly
Key Point
Diabetic retinopathy is a leading cause of blindness and visual loss however with appropriate screening, follow-up and timely treatment, the risk of blindness can be reduced by more than 90%. Most patients who get themselves in trouble haven’t been attending their diabetic eye checks. With regular checkups, we can see the changes happening in slow motion and treatment can be commenced at an early stage, giving you the best chance of maintaining good vision throughout your life.
Contact us to get help with any questions you may have, or support you may need.

